Enjoy Mill Valley
An Absolute Game-Changer: 2024 Mill Valley Music Fest Is Set to Become First-Ever U.S. Festival to Operate Entirely on Mobile Zero-Emission Batteries, Thanks to a Groundbreaking Partnership with Mill Valley-Born Moxion Power
“This crucial leap forward for the Mill Valley Music Festival comes at a critical moment in our community, as City of Mill Valley leaders, the Mill Valley Chamber, local businesses and a multitude of organizations take an all-hands-on-deck approach to reduce the burdens of climate change,” Jim Welte, executive director of the Mill Valley Chamber. “Our City has identified reducing greenhouse gas emissions as a major reduction strategy, along with renewable energy, energy efficiency, EV infrastructure, green building and waste reduction.”
Sample the Best of Mill Valley Featuring Local Artisans, Muralists, Jewelry Makers, Clothing Designers & Apparel Shops, Along With Local Restaurants, the Debut of Wine Valley, Arts & Crafts Activities, Nonprofit Orgs & Much More!
Beyond the highly-anticipated 2024 music lineup that features headliners Fleet Foxes (Saturday) and Greensky Bluegrass (Sunday), and among other acts like Thee Sacred Souls, Margo Price, Fruit Bats, St. Paul & the Broken Bones, and Rebirth Brass Band, Mill Valley Music Festival will again host a massive outdoor vendor village featuring many of the NorCal region’s best artisans, creatives, and designers as well as important community organizations and nonprofits.
Hometown Hero: On the Eve of the 2024 Mill Valley Music Fest, Legendary Rocker Sammy Hagar Is Honored With a Star on the Hollywood Walk of Fame!
“Being honored like that in front of my family and more friends than I thought I had, touched my heart so there is no word that can come close to saying what I felt and am still feeling,” Hagar said. “The amount of Redheads that showed up was mind blowing to the committee as well who said it was one of the best turnouts ever.” The event included appearances by Guy Fieri, Michael Anthony, John Mayer and Chad Smith, among many more.
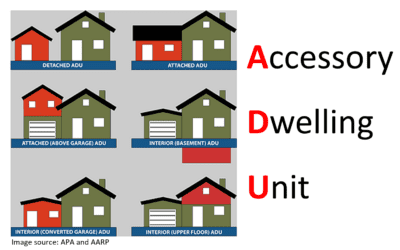
ADU Marin to Work With Cities to Provide Information on Developing the Apartments, Also Known as Granny Flats or In-Law Units
ADU Marin is working with officials in San Anselmo, Mill Valley, Fairfax, Larkspur, Sausalito, Novato, San Rafael, Corte Madera, Ross and the county to provide information on developing the apartments, also known as granny flats or in-law units, according to the Main Independent journal. The organization launched a website, ADUMarin.org, on April 1. A series of recorded webinars featuring local building and planning officials has been uploaded to the site.
Dipsea Race Foundation Hosts Hall of Fame and Scholarship Ceremony Dinner – June 7th, Spinnaker Restaurant
The event will also feature the 2024 Hall of Fame Induction of Norman Pease – 40 Consecutive Dipsea Races, and a celebration of Edda Stickle, Dipsea Race CFO and Co-Founder Dipsea Kidz Program. The Dipsea Foundation awards scholarship of $5,000 to college bound high school seniors who have participated in or volunteered for the Dipsea race. Awards are based on financial need, an essay, community service, leadership, athletic performance, and academics.
Marin JCC Hosts Shufuni: Look at Me – Music and Stories from Israel – May 16th, 7pm
Shufuni was established in 2022 to promote young artists coming from Sderot and the Gaza envelope area, with a goal to offer different types of events and platforms aimed at exposing the public to the unique voice of Israel’s southern communities. Current members include folk singer/songwriter Daniel Weiss, soul-folk singer Linor Ein Gedi, guitarist, drummer and music educator Rotem Meir Levi, and performer Mira Semandoyev, who recently appeared in the finals of the Israeli Idol show, Hakochav Haba.
Madrona Bakery Owners Look to Serve Up a Weekend of Deliciousness at 2024 Mill Valley Music Fest – May 11+12!
Now they’re ready for the next giant leap forward, as they’ll be serving an array of tasty treats at the 2024 Mill Valley Music Fest. What should MVMF-goers expect from Madrona? Quick breads like biscuits, scones, banana bread, cookies and foccacia – “a nice thing to tuck in your pocket,” Aron says. They’ll also be serving the always-delicious Four Barrel Coffee, including Iced Coffee and Iced teas via the Leaves and Flowers brand.
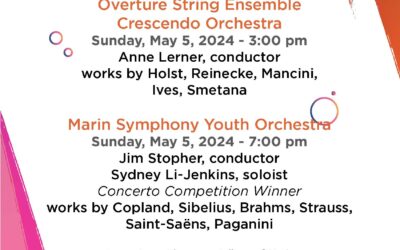
Marin Symphony Youth Orchestra Eyes a Summer Trip to Austria in 2025 to Play at Three Different Venues – They’re Seeking Raffle Donation to Support Their Fundraising
Marin Symphony Youth Orchestra is hoping to raise funds to help support this trip for everyone (there are students that are part of this group that are from lower socioeconomic background and are supported by the Marin Symphony leadership. The orchestra is seeking donations for raffles, donating for advertisement on the brochures for the three concerts that the kids have per year, and donations.
Upcoming Events in Mill Valley
#enjoymillvalley
Mill Valley in the Media
THE MISSION OF THE MILL VALLEY CHAMBER OF COMMERCE
To foster a vibrant community, we promote, inform, engage, and advocate for our members. We do this by creating events and content, championing vitality and equity, coaching and connecting members to spark opportunity and continuously improve our organization.
Enjoy Mill Valley is your community hub for all things MV
Explore
Events
Explore Membership
Music Festival
2024
Advertise With Us
Mill Valley Chamber of Commerce & Visitor Center
85 Throckmorton Avenue
Mill Valley, CA 94941
415.388.9700
Hours
Tuesday, Thursday, Friday & Saturday
noon - 4pm
info@millvalley.org